Recreational Therapy Month
February is Recreation Therapy Month, a chance to celebrate the talented recreation therapists and recreation therapy assistants that help so many Glenrose patients achieve their goals. There are 18 recreation therapists and 12 recreation therapy assistants employed at the Glenrose, plus casual staff that support as needed.
But what exactly does a recreation therapist do?
Shannell has been working as a recreation therapist at the Glenrose Hospital for the last three years. Below, she explains the role of a recreation therapist and details what the work involves.
Q&A with Shannell, Recreation Therapist, Glenrose Rehabilitation Hospital
What does a recreation therapist do?
Because we work in a rehab setting, our role at the hospital is essentially trying to remove any barriers to meaningful recreation and leisure for our patients. We often see this arise with a new diagnosis, which is why they’re in the hospital, or with an ongoing physical, emotional, cognitive or social limitation. Our goal is to work with our patients and our clients to maintain and improve overall health, but also quality of life long term.
Why did you choose to become a recreation therapist and what did your education path look like?
I was attracted to the human aspect. I have always been looking for a career in healthcare and chose recreation therapy specifically because of the unique hands-on role. I love the fact that you get to work with patients as they heal and discover new and improved versions of themselves. My mom is a nurse at a long-term care facility and I grew up volunteering with recreation therapy staff there, which is how I found my calling.
As far as schooling, I attended the University of Alberta. I have a Bachelor of Arts and Recreation, Sport and Tourism, with a focus on therapeutic recreation.The last part of my degree included the completion of a professional practicum, which I did here at the Glenrose. And ever since then, I’ve been working here, first as a casual, and now as a part-time staff. I’ve had the chance to work in every service area, from pediatrics, outpatient units, all the way up to geriatric psychiatry, where I work right now. I’ve gotten to see how recreation therapy can help any person, with any diagnosis, and any walk of life.
What does a typical day look like for you?
I am an inpatient recreation therapist which means that all my patients are staying overnight at the Glenrose. I start at my desk at the hospital, and will look through my patient list for that day. Then, I have team rounds with our interdisciplinary team of occupational therapists, physiotherapists, social workers and dieticians. I also work with psychiatrists in my unit, because it is a geriatric psychiatry unit. We go to the doctors and talk about the patients’ progress here at the hospital, what we should continue working on and what their goals are for the community. Based on those conversations, I’ll then move on to actual patient-centered care, which includes a lot of hands-on assessments.
When a patient is new to the hospital, they get a full recreation therapy assessment where we learn about their history in the community, what their previous activities were, if they have any goals for new activities, or exploring new pursuits, and then we work with them to make a plan for access in the community. This might include something like a senior centre, an adult day program, rec center, or an online activity they can access from their home. We help handle transportation, access to facilities and all of the community planning, which I think is my favorite part of the job.
I’ll also work with patients in a hands-on setting, facilitating different groups. At the Glenrose, we have many talented recreation therapy assistants that work alongside the therapists and do a lot of the hands-on work with the patients, based on their goals. For example, if a patient wanted to learn guitar, we would take the guitar to work one-on-one in their room to accomplish their goal, whether that means learning a new song or determining how they can increase the range of motion after extreme arthritis. A big part of my day is the patient-centered care assessments and future planning. At the end of the day, I like to return emails to individuals in the community who are working with my patients and chart my patients progress—what they said they enjoyed and what they want to continue working on. I always make a plan for the next day so I can hit the ground running first thing in the morning. It’s very busy, very action-packed, but I wouldn’t have it any other way!
What’s it like when a patient achieves their goals?
I think that’s a unique part of recreation therapy, you get to see your patients’ progress. Oftentimes when they come into the hospital they’re not in the best place, and by the time they leave, they have so much appreciation for themselves for either rediscovering a sense of self or finding a new way to take pieces of themselves that are still there, despite any impairment, and using that to cultivate a new life in the future.
What are some of the unique parts of the Glenrose recreation therapy program?
We have an aquatic facility on the main floor of the hospital where patients can work on things such as water walking or swimming. Some patients might need different adaptations, such as a pool lift to get them in and out of the pool, especially if they’ve had a diagnosis or an impairment that impacts different parts of bodily functions, like a spinal cord or brain injury. Prior to COVID, we were even running an aquasize class in our outpatient division. We also have a kayak in our pool, which allows patients to practice getting in, moving back and forth and getting out with their new body or different barriers. We have fishing in the pool as well! If a patient is looking to get back to fishing again, we can block off parts of the pool and help them get back to that. I think it is so cool that you can go fishing in the middle of a hospital!
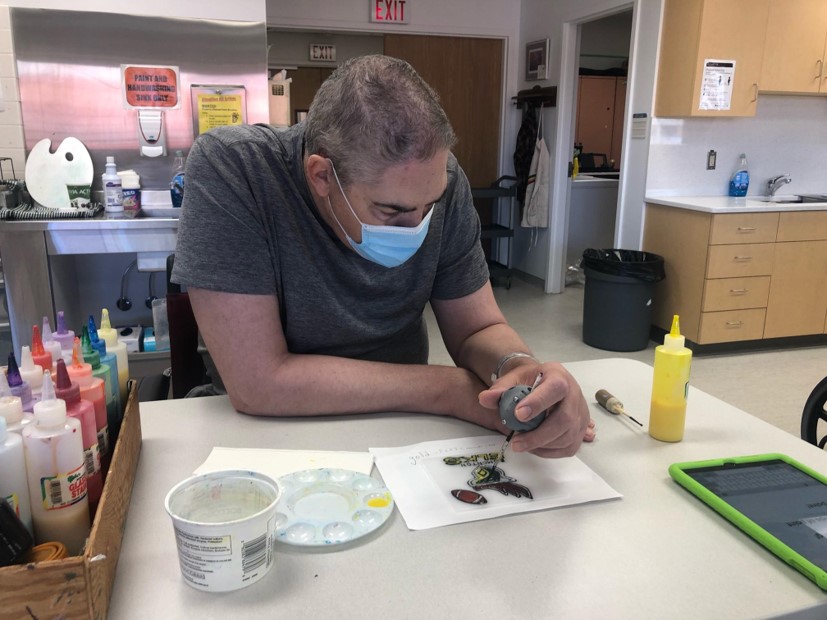
We also focus on using technology, including iPads and a Nintendo Switch. Patients of any age range can work on functional skills if they want to get back to playing games with friends or are looking for cognitive stimulation. We recently had a project to create adaptive tools for our patients using a 3D printer. We were able to create different adaptive aids, including knitting handles for patients with decreased range of motion or functional grip. Patients can actually use this device to help them knit. There are also ones for sanding wood, painting and holding a pen. We’ve used these adaptive aids a lot with patients in the art room, a space where we work on creative pursuits, and it helps patients who have decreased function in their hand after a brain injury or stroke paint as though they were painting with their old hands, which is really unique.
One thing I’m seeing with older adults here at the Glenrose is an ongoing need for socialization and stimulation. Having spent almost two years in the pandemic, a lot of seniors and older adults have felt isolated from their communities and their friends. When they come into care they’re looking for ways that they can resume that meaningfully when they go home. To support that, we work on a lot of cognitive simulation, typically through a program called Fit Minds. It is a program that only the Glenrose Hospital’s recreation therapists are licensed to facilitate. It focuses on five different areas of cognition that really help patients maintain their cognition in our care and also when they leave. Additionally, it’s a social program where they have a chance to make connections, meet their co-patients and bounce ideas for their rehab journey off of others in our care. Those are just a few areas that I think we really excel at.
The Glenrose is very unique because we have one of the largest rehabilitation departments, not only in our province, but across Canada. We have a lot of talented multifaceted therapists and assistants, who are always working to create the highest standard of care that mirrors our mission and our values.
What’s the best part of your job?
My favorite part is the ability for connection. With recreation therapy you have the chance to connect individuals to their old leisure activities, but also help them explore new activities. They can do activities themselves, or with their friends and their family. It gives them the confidence to make and maintain those connections, both when they’re here with us, and also in the community when they go to programs or rec centres.That connection to their community and finding ways to stay healthy and engage in a way that’s meaningful and keeps them integrated, is very specific to recreation therapy.
What is the hardest part of your job?
Right now, with COVID, the hardest part has been adaptability and flexibility. Before the pandemic we focused a lot on activities that gathered us together and involved sharing materials: a communal art project, shuffleboard, or group activities in the pool. We had to stop most of those at the start of the pandemic, and although they’ve resumed in some way, it’s really not the same as it was pre-COVID. Luckily, as recreation therapists we are all very adaptable. Our patients still are getting a high level of benefit and have very positive feedback despite COVID-19 and the ongoing protocols that we follow.
What do you think people might not know about recreation therapy?
Recreation therapy is so much more than play. When people think about recreation they often navigate to fun and play. But recreation therapy is so much more than that. Recreation therapists are very high functioning health care professionals who are helping patients set goals and achieve those goals. We work as coaches and supporters alongside patients in their rehab journey. And we help patients come out as the best version of themselves at the end of the day. And although we use activities like recreation leisure that are often meaningful and enjoyable, we still find ways to have that therapeutic rehabilitative aspect in a way that’s just a bit unique.
Recreational Therapy Month takes place every February